According to the NHS, seasonal affective disorder, or S.A.D, is “a type of depression that comes and goes in a seasonal pattern.”
They explain that the condition can be known as "winter depression", because the darker, colder weather in winter can bring on more obvious and extreme symptoms - though it’s also possible for S.A.D sufferers to experience their symptoms more acutely in the summer and find that the winter actually relieves them somewhat.
The team at Holiday Gems recently led a 2000 respondent survey into depression and sadness around winter and Christmas time, and undertook extensive seasonal affective disorder research. You can discover more about their findings below.

- According to the NHS, 1 in 15 people suffer from S.A.D between the months of September & April
- According to our survey, only 12% of people are completely aware, and know a lot about S.A.D
- Only 5% of respondents said that they feel the happiest in the winter, with the majority saying that they feel the happiest in the summer
- Almost 1 in 5 people with mental health issues have been prescribed antidepressants due to feelings brought on by Christmas time
How Many People are Affected by S.A.D?
Seasonal affective disorder is a relatively common condition, with around 1 in 15 individuals reported to be suffering from it between September and April.
28% of our survey’s respondents said that they currently have a mental health condition, or have had one in the past. 11% of members of this particular group also said that they suffered from S.A.D or “winter blues”.
Seasonal Affective Disorder Symptoms
The NHS lists common seasonal affective disorder symptoms as:
- a persistent low mood
- a loss of pleasure or interest in normal everyday activities
- Irritability
- feelings of despair, guilt and worthlessness
- feeling lethargic and sleepy during the day
- sleeping for longer than normal and finding it hard to get up in the morning
- craving carbohydrates and gaining weight
For some people, these symptoms can be severe and have a significant impact on their day-to-day activities.
What Causes S.A.D?
While the condition itself is still being studied and there are currently no definitive findings regarding its scientific and medical causes, it has been regularly theorised that it is triggered by a reduction of exposure to sunlight throughout autumn and winter - during which days are shorter.
This lack of sunlight could potentially cause the hypothalamus - a gland within the brain which is located almost right in the centre and keeps various conditions within the human body constant - regulating our temperature, hunger levels and blood pressure. It also manages feelings of stress.
What’s more, if the hypothalamus is not working correctly, it is likely to negatively affect:
- Production of melatonin – melatonin is a hormone that makes you feel sleepy; in people with SAD, the body may produce it in higher than normal levels.
- Production of serotonin – serotonin is a hormone that affects your mood, appetite and sleep; a lack of sunlight may lead to lower serotonin levels, which is linked to feelings of depression.
- The body's internal clock (circadian rhythm) – your body uses sunlight to time various important functions, such as when you wake up, so lower light levels during the winter may disrupt your body clock and lead to symptoms of SAD.
Seasonal Affective Disorder treatments
If you believe that you might be suffering from SAD, you should consider making an appointment to see your GP.
According to the NHS, there are a number of options to help improve SAD symptoms, ranging from steps you can take yourself, to prescribed medication.
Trying to get as much natural light as possible is important. Maybe go for a walk on your lunch break or sit near a window when you’re inside.
The NHS also recommends taking regular exercise, especially outside in daylight, as well as eating a healthy, balanced diet.
It is also advised that you should try to manage your stress levels and attempt to steer clear of stressful situations.
Another form of treatment is light therapy. This involves a special lamp called a light box being used to simulate sunlight and help to improve mood.
Someone suffering from SAD would usually sit by the box for around 30 minutes to an hour each morning.
It is thought the light helps to increase the production of serotonin in the brain and reduces the production of melatonin.
GPs can also recommend attending cognitive behavioural therapy sessions. This course of treatment helps to change how we think and behave in certain situations, in order to improve how we feel.
Counselling is another option, which involves talking to a trained counsellor about your problems and feelings.
In severe cases of SAD, GPs can prescribe antidepressants which help to improve your mood by increasing the level of serotonin in your brain.
A combination of treatments can also be used, with your GP able to recommend what’s best for you.
How Many People Know About S.A.D?
The results of Holiday Gems’ survey reveal that only approximately 12% of people are fully aware of the existence of seasonal affective disorder, even though the NHS estimates that 1 in 15 people across the UK actually suffers from it.
Almost 10% of respondents had never heard of S.A.D before and knew absolutely nothing about it at all.
Happiness in the Winter Months
Holiday Gems’ study included research into peoples’ happiness levels throughout the winter months. Read on for our findings.
General Happiness and Productivity in Winter
Only 5% of our survey’s respondents said that they felt happiest in winter - compared to the 46% who said that their mood was best in summer, representing a considerable majority.
We found that 55% felt unhappier in the months between November and February, with 57% explaining that their low mood was caused by a lack of sunlight in winter.
Sleep problems also appeared to be exacerbated by a seasonal change, with 27% of those who took part in our study saying that they got less sleep during winter and 56% admitting that they struggled to get out of bed in the morning in winter. Sleeping badly is a contributing factor to being diagnosed with S.A.D.
There was also a quantifiable rise in feelings of lethargy, with 57% of people saying that they felt less productive and motivated in the winter months.
Contributing Factors to Unhappiness in Winter
See the chart below for a few of the reasons why people said they felt unhappy throughout the darker, colder months of the year:
- Cold weather: 58%
- Dark mornings: 60%
- Loss of sleep: 18%
- Financial worries over Christmas: 25%
- Loneliness: 14%
- General stress: 23%
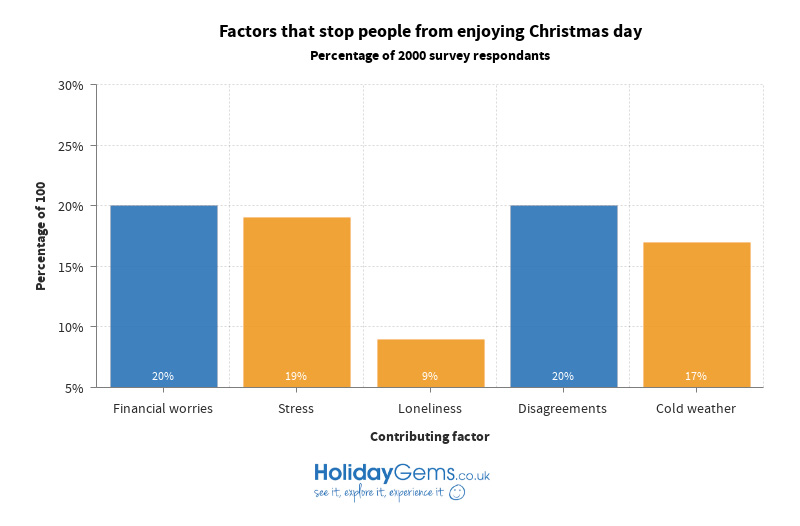
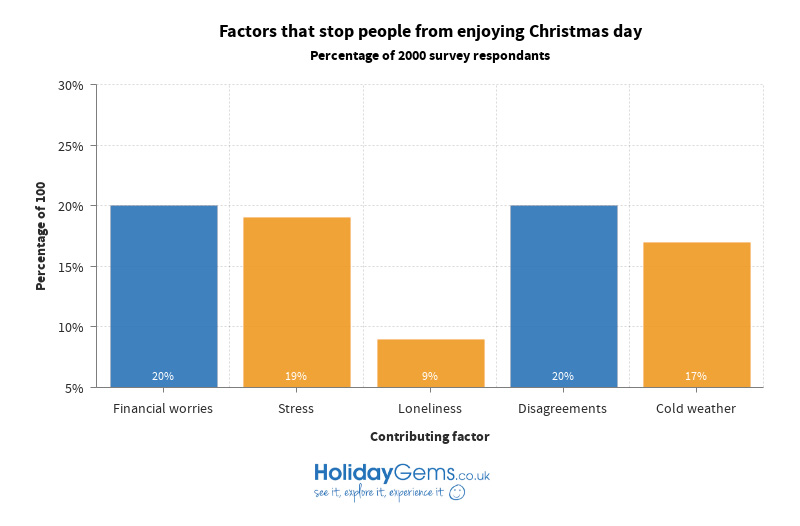
Happiness on Christmas Day
Our respondents revealed that the most wonderful time of the year can, in reality, prove to be a far less joyous occasion for some. 20% of them explained that their financial worries prevented them from enjoying Christmas day, while the same number also struggled with disagreements they had with friends, family members or others around this time. 19% admitted to suffering from levels of stress that ruined their experience of the festive period and 17% could not enjoy themselves at Christmas because of the cold. 13% said that they experienced lack of sleep to such an extent that Christmas was not enjoyable for them, and the same number found that work stress irreversibly undermined their Christmas cheer. Bad memories made 12% of respondents unhappy at Christmas, and loneliness affected 9%.
Seasonal Mental Health Statistics

Of the respondents who said they’d had a mental health condition at some point in their life, 47% mentioned that the colder, darker months exacerbated the symptoms of this condition. 16% of the same demographic said that Christmas makes their symptoms worse, and 18% had been prescribed antidepressants due to negative feelings at this particular time of year.
Out of our whole group of respondents, only 44% said that they truly liked Christmas day.
11% of our respondents said that they had seasonal affective disorder.
General Mental Health in the UK
Over 1 in 4 people who responded to our survey said that they currently have a mental health condition, or have had one in the past. Of these individuals, 79% had been diagnosed as such by a doctor, and 73% said that they had received professional help for the condition.
Only 22% of those who received professional help said that it was very effective, and the same number said that they would not visit a doctor about their condition because they did not want to admit that there might be a problem. 15% of respondents who had been affected by a mental health condition said that they had been put off getting professional help because they had used services before and found them to be poor.
Antidepressant Usage in the UK
Around 64 million antidepressants were prescribed in the UK between the years 2016 and 2017.
Of our survey’s respondents, 81% of those who said they had experienced a mental health condition took antidepressants, but only 30% of this group said that their antidepressants were very effective. 17% said that their antidepressants were not effective at all.
15% admitted that they took antidepressants that had not been prescribed to them, while 27% took other medication alongside antidepressants to manage their mental health.
37% had decided to turn to herbal remedies to help manage their mental health instead of antidepressants.



 My Booking
My Booking